Authored by RJ Tesi via RealClearScience,
Alzheimer’s disease (Alzheimer’s) is conceptualized as a progressive consequence of two hallmark pathological changes in gray matter, in particular, extracellular amyloid plaques and neurofibrillary tangles. However, over the past several years, neuroimaging studies have implicated micro and microstructural abnormalities in white matter in the risk and progression of Alzheimer’s, suggesting that in addition to the neuronal pathology characteristic of the disease, white matter degeneration and demyelination are crucial features of patients living with the disease. A shift to focus on white matter abnormalities, rather than gray matter, can open up critical new avenues in Alzheimer’s pathology and could be potential treatment targets.
White matter vs. gray matter
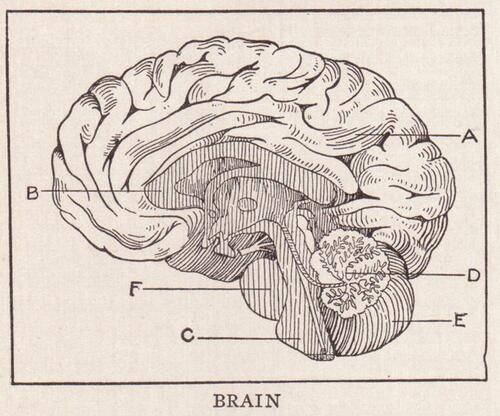
The brain’s gray matter is mainly composed of neuronal cell bodies. Nerve cells in the gray matter are where memories are stored. Networks of nerve cell bodies process information in the brain. These neuronal networks are necessary for thinking, speaking, and most activities. White matter is made up of myelinated axons.
White matter disease is the degeneration of tissue in the largest and deepest part of the brain. White matter tissue contains millions of nerve fibers, or axons, that connect other parts of the brain and spinal cord and signal your nerves to communicate to one another. This 'talk' helps individuals think fast, walk straight, and perform other important cognitive functions. When diseased, the myelin, a fatty material that protects fibers in the brain, and the axons stop working and the brain and body halt normal functions.
Growing research supporting Alzheimer’s as a white matter disease
The observation that white matter abnormalities are characteristic of Alzheimer’s is relatively new. While changes to the gray matter in the pathogenesis of Alzheimer’s are well known and continue to be heavily investigated, the neuropathology of white matter abnormalities still remains mysterious and is mainly attributed to cerebral small vessel degeneration, inflammatory events, as well as loss of myelin and axonal fibers. However, white matter changes have been shown to develop very early, in prodromal phase (pre-Alzheimer’s) and precede the onset of clinical symptoms of dementia, underscoring the importance of their further investigation and focus.
A neuroimaging study in 2020 identified white matter hyperintensities, a significant contributor to Neuropsychiatric symptoms (NPS), such as apathy, irritability and depression, to be present in subjects evaluated with Alzheimer’s. Another recent study demonstrated that co-morbidities have an impact on white matter integrity in individuals living with AD and that early alterations in genes linked to myelin proteins in white matter occur in AD cases. These are just a couple recent examples of the growing data that support the vital role white matter abnormalities present in the development of Alzheimer’s.
The fact that most dementia remains incurable—including the cortical dementia of Alzheimer’s that continues as such a formidable threat to medicine and society—calls out for a new paradigm that may reveal new avenues to an effective response. Alzheimer’s as a white matter disease may stimulate such novel thinking, and can serve in a theoretical sense to broaden the clinician’s perspective in approaching dementia and its origins.
New hope for Alzheimer’s disease treatment
Historically, science hasn’t paid as much attention to our brain’s white matter as its gray matter.
We now know how important white matter is to our overall brain health and cognitive ability, as well as how declines in white matter structure are correlated with impairments in brain function. In the broadest sense, dementia must arise from dysfunction in or damage to neurons in the brain. However, the details of where, when and how the cognitive disturbance arises are crucial. Just as neuronal cell body pathology within gray matter is important, so is disease involving the segments of neurons within the white matter and their supporting structures.
Heightened consideration of white matter as a specific therapeutic target raises many new possibilities for Alzheimer’s treatment. Emerging possibilities for the treatment of white matter disorders can help reduce the burden of dementia that results from long-term consequences of myelin damage or dysfunction. An adaptation and adjustment to focus on white matter abnormalities, rather than gray matter in Alzheimer’s patients, opens promising possibilities for the science community to develop effective treatments for Alzheimer’s patients and potentially take steps forward in identifying a possible cure.
Authored by RJ Tesi via RealClearScience,
Alzheimer’s disease (Alzheimer’s) is conceptualized as a progressive consequence of two hallmark pathological changes in gray matter, in particular, extracellular amyloid plaques and neurofibrillary tangles. However, over the past several years, neuroimaging studies have implicated micro and microstructural abnormalities in white matter in the risk and progression of Alzheimer’s, suggesting that in addition to the neuronal pathology characteristic of the disease, white matter degeneration and demyelination are crucial features of patients living with the disease. A shift to focus on white matter abnormalities, rather than gray matter, can open up critical new avenues in Alzheimer’s pathology and could be potential treatment targets.
White matter vs. gray matter
The brain’s gray matter is mainly composed of neuronal cell bodies. Nerve cells in the gray matter are where memories are stored. Networks of nerve cell bodies process information in the brain. These neuronal networks are necessary for thinking, speaking, and most activities. White matter is made up of myelinated axons.
White matter disease is the degeneration of tissue in the largest and deepest part of the brain. White matter tissue contains millions of nerve fibers, or axons, that connect other parts of the brain and spinal cord and signal your nerves to communicate to one another. This ‘talk’ helps individuals think fast, walk straight, and perform other important cognitive functions. When diseased, the myelin, a fatty material that protects fibers in the brain, and the axons stop working and the brain and body halt normal functions.
Growing research supporting Alzheimer’s as a white matter disease
The observation that white matter abnormalities are characteristic of Alzheimer’s is relatively new. While changes to the gray matter in the pathogenesis of Alzheimer’s are well known and continue to be heavily investigated, the neuropathology of white matter abnormalities still remains mysterious and is mainly attributed to cerebral small vessel degeneration, inflammatory events, as well as loss of myelin and axonal fibers. However, white matter changes have been shown to develop very early, in prodromal phase (pre-Alzheimer’s) and precede the onset of clinical symptoms of dementia, underscoring the importance of their further investigation and focus.
A neuroimaging study in 2020 identified white matter hyperintensities, a significant contributor to Neuropsychiatric symptoms (NPS), such as apathy, irritability and depression, to be present in subjects evaluated with Alzheimer’s. Another recent study demonstrated that co-morbidities have an impact on white matter integrity in individuals living with AD and that early alterations in genes linked to myelin proteins in white matter occur in AD cases. These are just a couple recent examples of the growing data that support the vital role white matter abnormalities present in the development of Alzheimer’s.
The fact that most dementia remains incurable—including the cortical dementia of Alzheimer’s that continues as such a formidable threat to medicine and society—calls out for a new paradigm that may reveal new avenues to an effective response. Alzheimer’s as a white matter disease may stimulate such novel thinking, and can serve in a theoretical sense to broaden the clinician’s perspective in approaching dementia and its origins.
New hope for Alzheimer’s disease treatment
Historically, science hasn’t paid as much attention to our brain’s white matter as its gray matter.
We now know how important white matter is to our overall brain health and cognitive ability, as well as how declines in white matter structure are correlated with impairments in brain function. In the broadest sense, dementia must arise from dysfunction in or damage to neurons in the brain. However, the details of where, when and how the cognitive disturbance arises are crucial. Just as neuronal cell body pathology within gray matter is important, so is disease involving the segments of neurons within the white matter and their supporting structures.
Heightened consideration of white matter as a specific therapeutic target raises many new possibilities for Alzheimer’s treatment. Emerging possibilities for the treatment of white matter disorders can help reduce the burden of dementia that results from long-term consequences of myelin damage or dysfunction. An adaptation and adjustment to focus on white matter abnormalities, rather than gray matter in Alzheimer’s patients, opens promising possibilities for the science community to develop effective treatments for Alzheimer’s patients and potentially take steps forward in identifying a possible cure.
Loading…




