President Joe Biden tested positive for COVID-19 again on Saturday, going through the phenomenon experts refer to as a Paxlovid rebound.
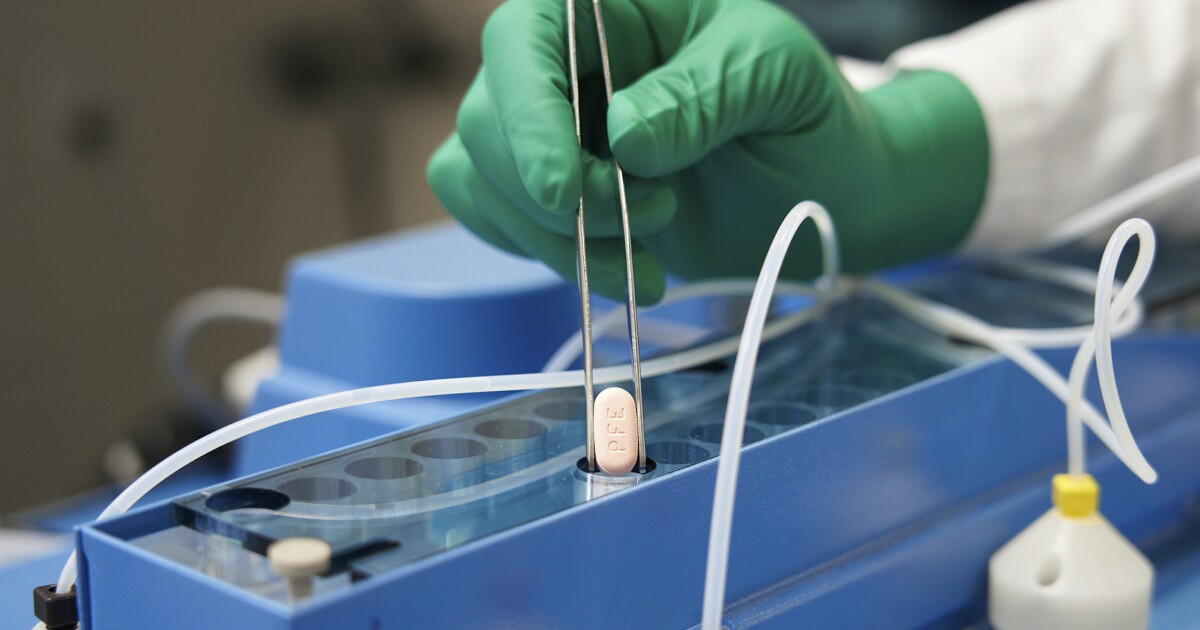
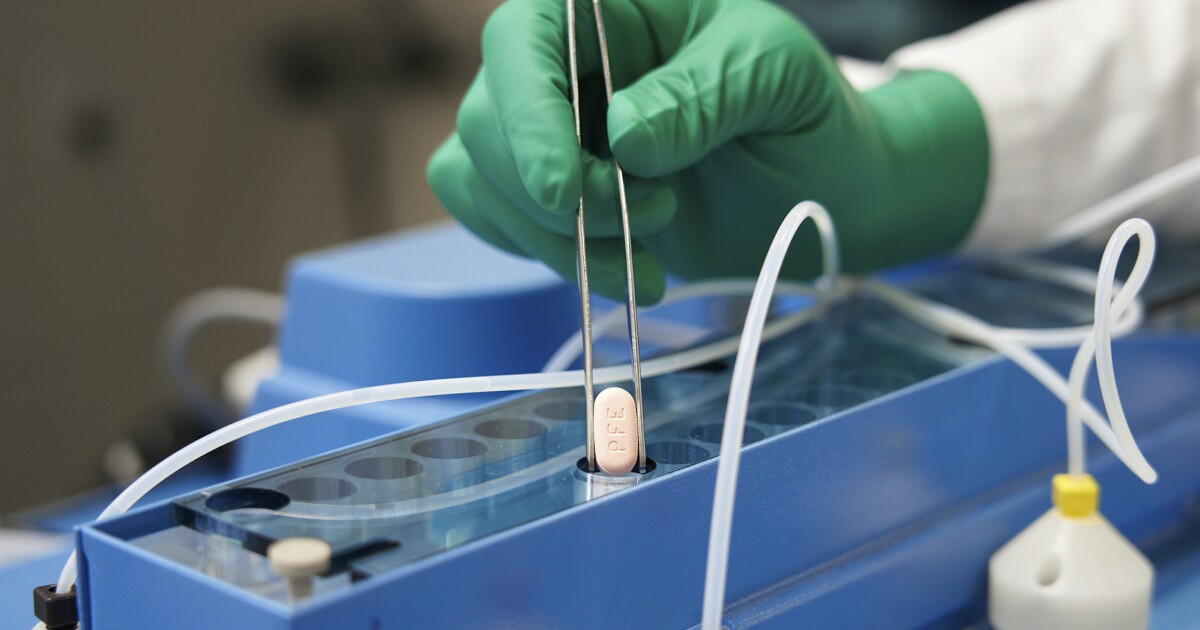
The president emerged from isolation on Wednesday after testing negative for the virus and completing a five-day course of Paxlovid, the antiviral treatment from Pfizer. White House physician Kevin O’Connor said in his Saturday announcement that Biden had increased his testing frequency because of the potential for a rebound infection. Biden continued to test negative on Tuesday evening, Wednesday morning, Thursday morning, and Friday morning, but the virus reemerged Saturday morning.
While the commander in chief is not exhibiting any symptoms, his positive test has sparked questions about how common Paxlovid rebounds really are. The Centers for Disease Control and Prevention issued a health advisory in May about the antiviral, which is being prescribed to over 40,000 people per day, addressing the rebound risk. The agency acknowledged that there were cases where the illness returned, but it cautioned that none of those affected had reported severe symptoms. The CDC also said there was no evidence that a second prescription of Paxlovid would resolve any rebound symptoms.
BIDEN RETESTS POSITIVE FOR COVID-19 IN ‘REBOUND’ INFECTION
With Biden experiencing no symptoms, Dr. O’Connor said it was not necessary for him to undergo a second course of the antiviral drug. Dr. Anthony Fauci, who also went through a Paxlovid rebound in June, took two courses of the treatment. Unlike Biden, though, his symptoms had resurfaced.
“When you look at the studies, it generally does not occur very often,” Fauci, who leads the National Institute of Allergy and Infectious Diseases and is the White House chief medical adviser, said of the potential for rebounds on MSNBC’s Morning Joe Tuesday. He noted, however, that “anecdotal cases” suggest rebounds are more common now than they were when clinical trials were conducted.
Dr. Ashish Jha, the White House COVID-19 response coordinator, said back in May that rebound infections were something they were “looking at very carefully,” adding that those cases were “not leading to people getting particularly sick.”
Jha offered a similar take at a White House press briefing last Thursday, saying: “If you look at Twitter, it feels like everybody has rebound, but it turns out there’s actually clinical data. If you look at major health systems that have given out Paxlovid to tens of thousands of people, rebound rates are around 5%. There are some studies that say it’s maybe 7-8%, some that say it’s 2%, but it’s in the single digits. So it happens; it’s not that frequent.”
“But here’s the key point,” he said. “When people have rebound, they don’t end up in the hospital. They don’t end up particularly sick. And the goal of Paxlovid is to keep people from getting seriously ill.”
Pfizer’s clinical trial for Paxlovid only showed about 1-2% of patients developing a rebound infection. Given reports of rebounds in more than 5% of Paxlovid patients, some experts have suggested the five-day course of the drug is too short to eradicate the virus fully.
Dr. Marc Siegel, a Fox News medical analyst and professor of medicine at New York University’s Langone Medical Center, said on the network that he was not surprised about Biden’s COVID-19 rebound.
“Paxlovid rebound for Biden is not a surprise. I was surprised when he ended quarantine after five days, even with two negative tests, because he still clearly had mild symptoms, including nasal congestion,” Siegel said. “What I think happens is that the Paxlovid stops the virus from reproducing, but when it wears off, there may still be some particles left, and they then start to reproduce again, and the test turns positive.”
A small study conducted by the Mayo Clinic in June found that just under 1% of COVID-19 patients developed rebound infections after taking Paxlovid. Researchers monitored 483 “high-risk” patients and reported that only “a handful” experienced rebounds, 0.8% in total. All of those who tested positive with the illness again eventually recovered, and the symptoms developed during the rebound were “generally mild.”
“We found that rebound phenomenon was uncommon in this group of patients. The four individuals who experienced rebound (symptoms) represent only 0.8% of the group, and all of them recovered quickly without additional COVID-directed therapy,” Dr. Aditya Shah, who led the Mayo Clinic study, said in a statement. He added that more studies were necessary to determine the reason for and frequency of Paxlovid rebounds.
CLICK HERE TO READ MORE FROM THE WASHINGTON EXAMINER
Speaking to NBC News last week, Shah cautioned that the frequency of rebound cases was difficult to track, noting that the real number of such instances “could be as high as 5-10%, but I don’t think it is as common as the general community is making it out to be.”
Researchers at the University of California San Diego School of Medicine released results of a similar study in June, which found that COVID-19 rebounds after taking Paxlovid appeared to stem from insufficient exposure to the antiviral drug.
“The goal of Paxlovid is to prevent serious illness and death, and so far, no one who has gotten sick again has needed to be hospitalized, so it’s still doing its job,” Dr. Davey Smith, who led the study, said. “We simply need to understand why the rebound happens in some patients and not others. More research is needed to help us adjust treatment plans as necessary.”







