A long-suppressed dread disease appears to be taking up permanent residence in America's Southeast, with Florida emerging as a principal hot spot.
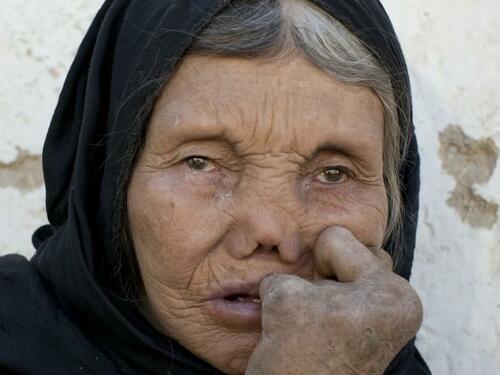
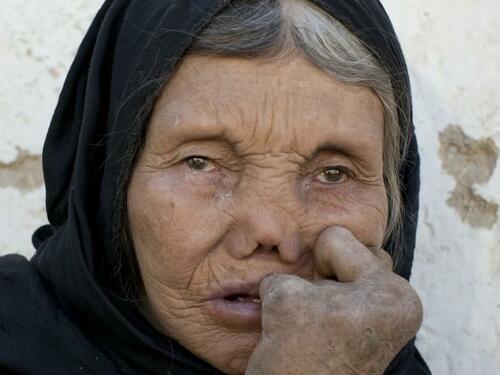
That disease is leprosy, also known as Hansen's disease. Caused by slow-growing bacteria, it can affect nerves, skin, eyes, and nasal lining. While early treatment can be highly effective, a neglected case can lead to crippling disfigurement, paralysis and blindness.
Cases in America most recently peaked in 1980, followed by a dramatic decline. Since 2000, however, cases have been gradually rising, and have doubled in the southeastern states, according to the Centers for Disease Control and Prevention. Central Florida accounts for nearly a fifth of all cases in the United States.
The numbers themselves aren't alarming yet -- eight cases in Florida in 2023. However, what's particularly concerning is that recent infections don't appear to have originated from foreign travel to high-risk countries like India, Brazil and Bangladesh.
“Florida has witnessed an increased incidence of leprosy cases lacking traditional risk factors. Those trends, in addition to decreasing diagnoses in foreign-born persons, contribute to rising evidence that leprosy has become endemic in the southeastern United States,” say the authors of a CDC report. "Endemic" describes a disease that regularly occurs in a given region. "Travel to Florida should be considered when conducting leprosy contact tracing in any state."
In 2020, six states accounted for 69% of the country's 159 cases of leprosy: Florida, California, Louisiana Hawaii, New York and Texas. The CDC spotlights the case of a 54-year-old man who contracted leprosy in 2022, with painful lesions and swelling:
“He denied any domestic or foreign travel, exposure to armadillos, prolonged contact with immigrants from leprosy-endemic countries, or connections with someone known to have leprosy. He has resided in central Florida his entire life, works in landscaping, and spends long periods of time outdoors.”

You read that right: where the spread of leprosy is concerned, the CDC says contact with armadillos could play a role. "A high percentage of unrelated leprosy cases in the southern United States were found to carry the same unique strain of M. leprae as nine-banded armadillos in the region, suggesting a strong likelihood of zoonotic transmission," say the CDC report authors. A Colorado State University study suggests that handling and eating armadillo meat is far more risky than casual contact.
Assuming you don't eat armadillos, you're far more likely to catch leprosy from a human: "Prolonged person-to-person contact through respiratory droplets is the most widely recognized route of transmission," says the CDC.
Prompt treatment with antibiotics is highly effective. The Health Resources & Services Administration says "patients become noninfectious after taking only a few doses of medication and need not be isolated from family and friends."
Thankfully, that means that, unlike what was done in previous times, lepers need not be exiled to colonies, as dramatized in the 1973 Steve McQueen movie, Papillon:
A long-suppressed dread disease appears to be taking up permanent residence in America’s Southeast, with Florida emerging as a principal hot spot.
That disease is leprosy, also known as Hansen’s disease. Caused by slow-growing bacteria, it can affect nerves, skin, eyes, and nasal lining. While early treatment can be highly effective, a neglected case can lead to crippling disfigurement, paralysis and blindness.
Cases in America most recently peaked in 1980, followed by a dramatic decline. Since 2000, however, cases have been gradually rising, and have doubled in the southeastern states, according to the Centers for Disease Control and Prevention. Central Florida accounts for nearly a fifth of all cases in the United States.
The numbers themselves aren’t alarming yet — eight cases in Florida in 2023. However, what’s particularly concerning is that recent infections don’t appear to have originated from foreign travel to high-risk countries like India, Brazil and Bangladesh.
“Florida has witnessed an increased incidence of leprosy cases lacking traditional risk factors. Those trends, in addition to decreasing diagnoses in foreign-born persons, contribute to rising evidence that leprosy has become endemic in the southeastern United States,” say the authors of a CDC report. “Endemic” describes a disease that regularly occurs in a given region. “Travel to Florida should be considered when conducting leprosy contact tracing in any state.”
In 2020, six states accounted for 69% of the country’s 159 cases of leprosy: Florida, California, Louisiana Hawaii, New York and Texas. The CDC spotlights the case of a 54-year-old man who contracted leprosy in 2022, with painful lesions and swelling:
“He denied any domestic or foreign travel, exposure to armadillos, prolonged contact with immigrants from leprosy-endemic countries, or connections with someone known to have leprosy. He has resided in central Florida his entire life, works in landscaping, and spends long periods of time outdoors.”

You read that right: where the spread of leprosy is concerned, the CDC says contact with armadillos could play a role. “A high percentage of unrelated leprosy cases in the southern United States were found to carry the same unique strain of M. leprae as nine-banded armadillos in the region, suggesting a strong likelihood of zoonotic transmission,” say the CDC report authors. A Colorado State University study suggests that handling and eating armadillo meat is far more risky than casual contact.
Assuming you don’t eat armadillos, you’re far more likely to catch leprosy from a human: “Prolonged person-to-person contact through respiratory droplets is the most widely recognized route of transmission,” says the CDC.
Prompt treatment with antibiotics is highly effective. The Health Resources & Services Administration says “patients become noninfectious after taking only a few doses of medication and need not be isolated from family and friends.”
Thankfully, that means that, unlike what was done in previous times, lepers need not be exiled to colonies, as dramatized in the 1973 Steve McQueen movie, Papillon:
[embedded content]
Loading…





