
Authored by Zachary Stieber via The Epoch Times (emphasis ours),
Advisers to the U.S. Food and Drug Administration (FDA) voiced support on May 18 for Pfizer’s maternal RSV vaccine even after several expressed concerns over premature births.

Outside experts on the Vaccines and Related Biological Products Advisory Committee unanimously said data from two trials run by Pfizer were sufficient to support the vaccine being effective at preventing RSV disease in infants. They also voted 10–4 in the affirmative when asked if the data from the trials were sufficient to demonstrate the safety of the vaccine.
The votes set up FDA clearance for what would be the first maternal vaccine for the respiratory syncytial virus, or RSV.
Pfizer’s vaccine, a recombinant protein subunit shot, targets the RSV A and RSV B subgroups in a 120 microgram dose that would be given to pregnant women in the second or third trimester. The goal would be to relay antibodies against RSV to fetuses, conferring protection that is supposed to last through the first year of life.
The vaccine was 81.8 percent efficacious through 90 days after birth against severe lower respiratory tract illness due to RSV. The efficacy dropped to 69.4 percent after another 90 days.
For any RSV-positive medically attended lower respiratory tract illness, the vaccine started at 57.1 percent efficacy and dropped to 51.3 percent over the same timeframe, according to data from a phase 3 trial that included about 3,500 vaccinated pregnant women.
The efficacy for medically attended lower respiratory tract illness from any cause was just 2.5 percent at 180 days and 5.1 percent at 360 days.
FDA staffers said in a briefing document that the trial showed “successful vaccine efficacy," and the advisers seconded that view with their unanimous vote.
But multiple experts expressed concerns about the risk of the vaccine causing premature births, a risk found in a similar product made by GlaxoSmithKline that prompted the company to halt testing in 2022.
In Pfizer’s trial, there were more premature deliveries in the vaccinated arm than the placebo arm—5.7 percent in the former versus 4.7 percent in the latter.
“That is hanging over this program,” Dr. Paul Offit, one of the FDA’s advisers, said during Thursday’s meeting.
The FDA declined to comment on the issue during the meeting, though staffers wrote in a brief that there was “potential uncertainty” regarding premature births.
Pfizer executives said Pfizer’s vaccine has important differences from the GlaxoSmithKline one, including the way they’re stabilized. They also acknowledged that there was “an overall significant difference in preterm births” between the arms but said the difference was not statistically significant and was driven primarily by data from sites in South Africa.
“I think we need to place all of this in context. As you’ve already heard, the overall results show no statistically significant difference. The results are driven by the upper- and middle-income countries with the high-income countries not showing this difference,” Dr. William Gruber, Pfizer’s senior vice president for vaccine clinical research and panelists, told panelists. “And as you’ve heard from us, as well as the FDA, there’s the real opportunity, then, to look at this during the period of pharmacovigilance, when we have larger numbers of women being vaccinated, to determine whether or not there is, in fact, any sort of a signal.”
“But the evidence to this point provides no real support when we take the totality of it based on the Pfizer vaccine for an increased risk of prematurity, and we can investigate that, again, post-approval,” he added later.
The quote drew criticism from Rep. Greg Murphy (R-N.C.), a doctor who criticized a similar comment made about Pfizer’s COVID-19 vaccine.
“Most drugs carry side effects. When considering maternal vaccinations, significant complications such as severe premature births or even pre-term and neonatal deaths may be present. The notion of vaccinating populations to determine whether or not there will be any side effects leads to a mistrust in the FDA, public health, and the medical community,” Murphy told The Epoch Times in an emailed statement.
Dr. Iona Munjal, a Pfizer senior director for vaccines, noted during the meeting that there were more deaths in the placebo group. “When you look at poor outcomes like death or poor neonatal outcomes in our study, we don’t see those poor outcomes,” she said. “And this is probably due to the fact that most of the infants are born very near term and not proximally related to the vaccine.”
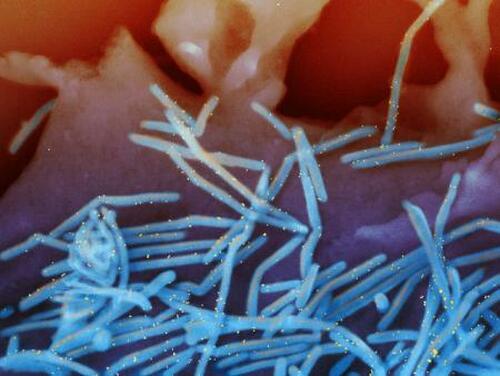
RSV
RSV peaks in the United States during the winter, with very low levels during the summer and fall. It primarily affects children under the age of 1, though it also impacts older children. The U.S. Centers for Disease Control and Prevention (CDC) estimates 100 to 300 children die each year from RSV, though a death certificate review for the 12 years ending in 2016 identified just 478 in that population, including 315 younger than age 1.
Approximately 68 percent of infants are infected before they turn 1, panel members heard, and U.S. officials say the vaccine would help curb a major reason for hospitalization.
The vaccine and others like it are “designed to overcome the shortcomings of previous efforts … [and] represent structural immunology and molecular engineering over empiric vaccinology against a respiratory virus that exacts its heaviest disease burden in the youngest and older adults,” Dr. David Kaslow, the director of the FDA’s Office of Vaccines Research and Review, told the panel.
The Pfizer vaccine efficacy for hospitalizations due to RSV was 67.7 percent at 90 days but dropped to just 33.3 percent at 360 days, according to the trial data.
Only one RSV vaccine is currently available in the United States. It is only for adults aged 60 and older.
Votes
Many panelists said they were convinced by the high efficacy data, despite concerns about the premature births.
“If the vaccine actually lives up to the data that we’ve seen today, I can guarantee that many infants and their parents will breathe easier in the coming years,” Dr. Jay Portnoy, one of the members, said.
Some said there’s a need for a vaccine.
“If there’s anything real there, we want to make sure we are aware of this. But this really does address a real, real strong need; there isn’t another option here for prevention,” Adam Berger, one of the panelists, said. “And it really could save a lot of lives. So I do think a lot of this is going to lie on the postmarketing requirements.”
The FDA lists required studies for drug and vaccine manufacturers to carry out in letters of authorization and approval.
Others echoed Pfizer in asserting that observational data, or looking at outcomes in women who receive the vaccine after it is cleared, would clear up whether premature birth is a side effect.
“Observational studies, as we go forward will fairly quickly give us an answer. If there is a problem there,” Dr. Arnold Monto, another member, said. “We learned how to bite the bullet and get things out during the SARS-CoV-2 vaccine approvals.”
Dr. Henry Bernstein, another member, said he had reservations due to not wanting another situation like the quick removal of a rotavirus vaccine following a spike in cases of intussusception, a life-threatening condition. Intussusception following vaccination “was not statistically significant until it was more widely used,” he said.
While all members said the efficacy data support licensure, Offit, Bernstein, Holly Janes, and Dr. Hana El Sahly said the safety data were not sufficient.
“If you’re in any sense risking premature births with this vaccine, I think there’ll be a big price to pay. And so I just don’t feel we have enough data to be reassuring,” Offit said.
“There was too much uncertainty,” Janes added. “And I’m uncomfortable with the notion of kicking the can down the road … toward post-marketing surveillance studies. I think it’s a bit different to rely on surveillance studies to sort of confirm what appears to be a safe product whereas here, I think the signals are such that the post-marketing surveillance data would be asked to refute what is sort of a potential hypothesis here, and I think that’s a higher bar.”
Authored by Zachary Stieber via The Epoch Times (emphasis ours),
Advisers to the U.S. Food and Drug Administration (FDA) voiced support on May 18 for Pfizer’s maternal RSV vaccine even after several expressed concerns over premature births.

Outside experts on the Vaccines and Related Biological Products Advisory Committee unanimously said data from two trials run by Pfizer were sufficient to support the vaccine being effective at preventing RSV disease in infants. They also voted 10–4 in the affirmative when asked if the data from the trials were sufficient to demonstrate the safety of the vaccine.
The votes set up FDA clearance for what would be the first maternal vaccine for the respiratory syncytial virus, or RSV.
Pfizer’s vaccine, a recombinant protein subunit shot, targets the RSV A and RSV B subgroups in a 120 microgram dose that would be given to pregnant women in the second or third trimester. The goal would be to relay antibodies against RSV to fetuses, conferring protection that is supposed to last through the first year of life.
The vaccine was 81.8 percent efficacious through 90 days after birth against severe lower respiratory tract illness due to RSV. The efficacy dropped to 69.4 percent after another 90 days.
For any RSV-positive medically attended lower respiratory tract illness, the vaccine started at 57.1 percent efficacy and dropped to 51.3 percent over the same timeframe, according to data from a phase 3 trial that included about 3,500 vaccinated pregnant women.
The efficacy for medically attended lower respiratory tract illness from any cause was just 2.5 percent at 180 days and 5.1 percent at 360 days.
FDA staffers said in a briefing document that the trial showed “successful vaccine efficacy,” and the advisers seconded that view with their unanimous vote.
But multiple experts expressed concerns about the risk of the vaccine causing premature births, a risk found in a similar product made by GlaxoSmithKline that prompted the company to halt testing in 2022.
In Pfizer’s trial, there were more premature deliveries in the vaccinated arm than the placebo arm—5.7 percent in the former versus 4.7 percent in the latter.
“That is hanging over this program,” Dr. Paul Offit, one of the FDA’s advisers, said during Thursday’s meeting.
The FDA declined to comment on the issue during the meeting, though staffers wrote in a brief that there was “potential uncertainty” regarding premature births.
Pfizer executives said Pfizer’s vaccine has important differences from the GlaxoSmithKline one, including the way they’re stabilized. They also acknowledged that there was “an overall significant difference in preterm births” between the arms but said the difference was not statistically significant and was driven primarily by data from sites in South Africa.
“I think we need to place all of this in context. As you’ve already heard, the overall results show no statistically significant difference. The results are driven by the upper- and middle-income countries with the high-income countries not showing this difference,” Dr. William Gruber, Pfizer’s senior vice president for vaccine clinical research and panelists, told panelists. “And as you’ve heard from us, as well as the FDA, there’s the real opportunity, then, to look at this during the period of pharmacovigilance, when we have larger numbers of women being vaccinated, to determine whether or not there is, in fact, any sort of a signal.”
“But the evidence to this point provides no real support when we take the totality of it based on the Pfizer vaccine for an increased risk of prematurity, and we can investigate that, again, post-approval,” he added later.
The quote drew criticism from Rep. Greg Murphy (R-N.C.), a doctor who criticized a similar comment made about Pfizer’s COVID-19 vaccine.
“Most drugs carry side effects. When considering maternal vaccinations, significant complications such as severe premature births or even pre-term and neonatal deaths may be present. The notion of vaccinating populations to determine whether or not there will be any side effects leads to a mistrust in the FDA, public health, and the medical community,” Murphy told The Epoch Times in an emailed statement.
Dr. Iona Munjal, a Pfizer senior director for vaccines, noted during the meeting that there were more deaths in the placebo group. “When you look at poor outcomes like death or poor neonatal outcomes in our study, we don’t see those poor outcomes,” she said. “And this is probably due to the fact that most of the infants are born very near term and not proximally related to the vaccine.”
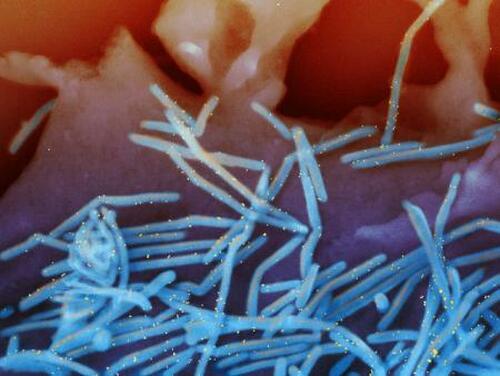
RSV
RSV peaks in the United States during the winter, with very low levels during the summer and fall. It primarily affects children under the age of 1, though it also impacts older children. The U.S. Centers for Disease Control and Prevention (CDC) estimates 100 to 300 children die each year from RSV, though a death certificate review for the 12 years ending in 2016 identified just 478 in that population, including 315 younger than age 1.
Approximately 68 percent of infants are infected before they turn 1, panel members heard, and U.S. officials say the vaccine would help curb a major reason for hospitalization.
The vaccine and others like it are “designed to overcome the shortcomings of previous efforts … [and] represent structural immunology and molecular engineering over empiric vaccinology against a respiratory virus that exacts its heaviest disease burden in the youngest and older adults,” Dr. David Kaslow, the director of the FDA’s Office of Vaccines Research and Review, told the panel.
The Pfizer vaccine efficacy for hospitalizations due to RSV was 67.7 percent at 90 days but dropped to just 33.3 percent at 360 days, according to the trial data.
Only one RSV vaccine is currently available in the United States. It is only for adults aged 60 and older.
Votes
Many panelists said they were convinced by the high efficacy data, despite concerns about the premature births.
“If the vaccine actually lives up to the data that we’ve seen today, I can guarantee that many infants and their parents will breathe easier in the coming years,” Dr. Jay Portnoy, one of the members, said.
Some said there’s a need for a vaccine.
“If there’s anything real there, we want to make sure we are aware of this. But this really does address a real, real strong need; there isn’t another option here for prevention,” Adam Berger, one of the panelists, said. “And it really could save a lot of lives. So I do think a lot of this is going to lie on the postmarketing requirements.”
The FDA lists required studies for drug and vaccine manufacturers to carry out in letters of authorization and approval.
Others echoed Pfizer in asserting that observational data, or looking at outcomes in women who receive the vaccine after it is cleared, would clear up whether premature birth is a side effect.
“Observational studies, as we go forward will fairly quickly give us an answer. If there is a problem there,” Dr. Arnold Monto, another member, said. “We learned how to bite the bullet and get things out during the SARS-CoV-2 vaccine approvals.”
Dr. Henry Bernstein, another member, said he had reservations due to not wanting another situation like the quick removal of a rotavirus vaccine following a spike in cases of intussusception, a life-threatening condition. Intussusception following vaccination “was not statistically significant until it was more widely used,” he said.
While all members said the efficacy data support licensure, Offit, Bernstein, Holly Janes, and Dr. Hana El Sahly said the safety data were not sufficient.
“If you’re in any sense risking premature births with this vaccine, I think there’ll be a big price to pay. And so I just don’t feel we have enough data to be reassuring,” Offit said.
“There was too much uncertainty,” Janes added. “And I’m uncomfortable with the notion of kicking the can down the road … toward post-marketing surveillance studies. I think it’s a bit different to rely on surveillance studies to sort of confirm what appears to be a safe product whereas here, I think the signals are such that the post-marketing surveillance data would be asked to refute what is sort of a potential hypothesis here, and I think that’s a higher bar.”
Loading…





